Brain tumours are complex and varied, with each type posing unique challenges. Understanding these types can help demystify neurological disorders and provide crucial insights for patients and their families. This guide aims to break down the complexities of brain tumours into digestible information, focusing on the primary types, their characteristics, and treatment options.
Brain tumours are abnormal growths
Brain tumours are abnormal growths of cells within the brain. While some tumours are benign, meaning they are non-cancerous, others are malignant, indicating they are cancerous. Tumours can originate in the brain (primary brain tumours) or spread from other parts of the body (metastatic brain tumours).
Primary brain tumours originate in the brain and can be either benign or malignant. They are classified based on the type of cell they originate from and the location within the brain.
Primary brain tumours
Primary brain tumours are classified according to the cells they arise from. This classification helps in understanding their behavior and potential treatment strategies. Tumours can stem from neurons, glial cells, or other types of cells within the brain. Each cell type gives rise to different tumour characteristics.
The location of a tumour
The location of a tumour within the brain can significantly influence symptoms and treatment options. Tumours in different brain regions can affect various neurological functions, leading to symptoms specific to those areas. For instance, a tumour in the cerebellum may impact balance, while one in the frontal lobe might affect personality or decision-making.
tumours are non-cancerous
While benign tumours are non-cancerous and usually have a slower growth rate, malignant tumours are cancerous and often aggressive. However, the location of a benign tumour in a critical brain area can still pose significant health risks. Malignant tumours, on the other hand, tend to spread more rapidly and require more aggressive treatment.
Gliomas are the most common type of primary brain tumour, accounting for about 30% of all brain tumours and 80% of malignant brain tumours. They arise from glial cells, which support nerve cells. There are several types of gliomas, including:
Astrocytomas develop
Astrocytomas develop from astrocytes, a type of glial cell. They can range from low-grade (slow-growing) to high-grade (fast-growing and aggressive). Low-grade astrocytomas may be treated with surgery alone, while high-grade astrocytomas often require additional treatments like radiation or chemotherapy. The prognosis for astrocytomas varies widely based on their grade and location.
Originating from oligodendrocytes, these tumours are generally slower-growing but can become more aggressive over time. Oligodendrogliomas often respond well to chemotherapy and radiation, especially if they contain a specific genetic mutation. Understanding the genetic profile of these tumours can aid in tailoring personalized treatment plans.
Ependymomas develop
Ependymomas develop from ependymal cells lining the ventricles of the brain and the central canal of the spinal cord. These tumours can occur at any age but are more common in children. Treatment usually involves surgery and radiation, and ongoing research is focused on improving outcomes for pediatric cases.
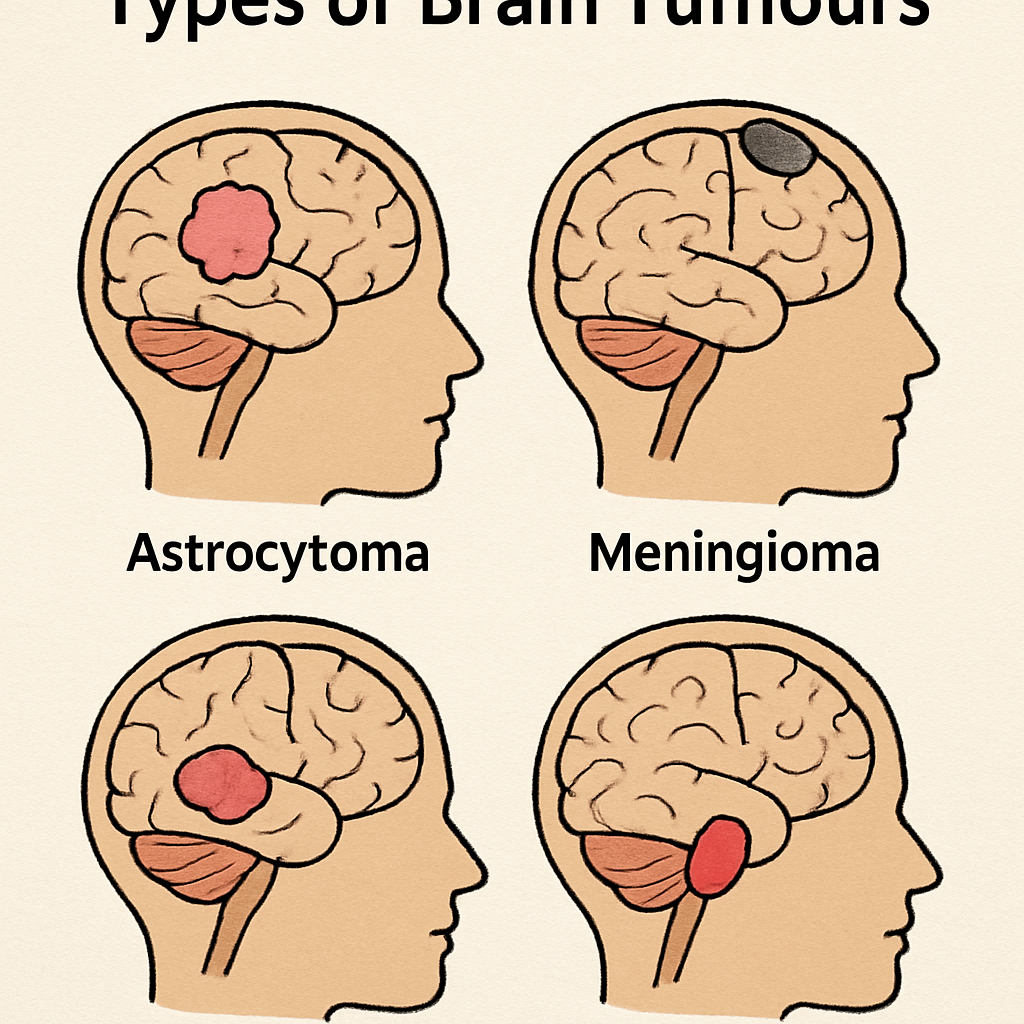
Meningiomas
Meningiomas develop from the meninges, the protective membranes covering the brain and spinal cord. They are typically benign and slow-growing but can cause symptoms by pressing on the brain or spinal cord.
Symptomatology of Meningiomas
Symptoms of meningiomas depend largely on their size and location. Small tumours might remain asymptomatic for years, while larger ones can cause headaches, vision changes, or seizures. Regular monitoring through imaging is often recommended for small, asymptomatic meningiomas.
Surgical Intervention
Surgery is the primary treatment for symptomatic meningiomas. The goal is to remove the tumour entirely, though complete resection may not always be possible due to its location. In such cases, partial removal is followed by regular monitoring or additional treatments.
Non-Surgical Treatments
For inoperable meningiomas or those that recur, radiation therapy is a common approach. Advances in radiation technology have improved the precision of treatments, minimizing damage to surrounding healthy tissues. In some cases, medications that target hormone receptors may also be considered, as some meningiomas are hormonally responsive.
Schwannomas
Schwannomas, also known as neurilemmomas, develop from Schwann cells, which insulate nerves. The most common type is the vestibular schwannoma, also known as acoustic neuroma, affecting the nerve responsible for balance and hearing.
Vestibular Schwannoma
Vestibular schwannomas primarily affect hearing and balance, leading to symptoms such as hearing loss, tinnitus, and dizziness. Early diagnosis is crucial for preserving hearing and balance functions. Treatment options vary based on the tumour’s size and growth rate.
Treatment Strategies
Observation is often recommended for small, asymptomatic schwannomas. For larger or symptomatic tumours, surgical removal or radiation therapy may be necessary. The choice between surgery and radiation depends on the tumour’s size, location, and potential impact on hearing.
Emerging Therapies
Research into targeted therapies for schwannomas is ongoing, focusing on molecular pathways involved in tumour growth. These therapies aim to slow tumour progression and are particularly valuable for patients with genetic conditions predisposing them to schwannomas.
Secondary Brain Tumours (Metastatic Tumours)
Secondary brain tumours, or metastatic brain tumours, originate from cancer cells that have spread to the brain from other parts of the body. They are more common than primary brain tumours and often originate from lung, breast, kidney, or melanoma cancers.
Common Origins
Metastatic brain tumours frequently arise from cancers of the lung, breast, kidney, and melanoma. The spread of cancer cells to the brain is a complex process involving the bloodstream or lymphatic system. Understanding the primary source of the cancer is crucial for effective treatment planning.
Diagnosis and Management
Diagnosis of metastatic brain tumours involves imaging studies and often a biopsy to confirm the origin of the cancer cells. Treatment typically includes a combination of surgery, radiation, and systemic therapies like chemotherapy or targeted agents, depending on the primary cancer type.
Palliative Care Considerations
For patients with advanced metastatic brain tumours, palliative care plays a critical role in managing symptoms and improving quality of life. This may involve pain management, management of neurological symptoms, and support for emotional and psychological well-being.
Symptoms of Brain Tumours
The symptoms of brain tumours can vary greatly depending on the tumour’s size, type, and location. Common symptoms include:
Headaches
Headaches associated with brain tumours are often severe and persistent. They may worsen with activities like coughing or changing positions. These headaches are typically more intense in the morning and may be accompanied by nausea or vomiting.
Seizures
Seizures are a common symptom of brain tumours and can occur in individuals who have never had seizures before. They vary in type and severity, ranging from focal seizures affecting a small part of the brain to generalized seizures affecting the entire brain.
Neurological and Cognitive Changes
Difficulty with balance and coordination, changes in personality or behavior, and memory problems are common neurological symptoms. These can affect daily functioning and quality of life, making early diagnosis and intervention crucial.
Sensory and Motor Symptoms
Nausea and vomiting, as well as vision or speech difficulties, may also occur. These symptoms are often related to increased pressure within the skull or specific areas of the brain being affected by the tumour.
Differential Diagnosis
These symptoms can also be caused by other conditions, so it’s important to consult a healthcare professional for a proper diagnosis. Differential diagnosis is essential to rule out other potential causes of these symptoms, such as infections, strokes, or other neurological conditions.
Diagnosing Brain Tumours
Diagnosing brain tumours involves a combination of medical history, physical examination, and specialized tests. These tests may include:
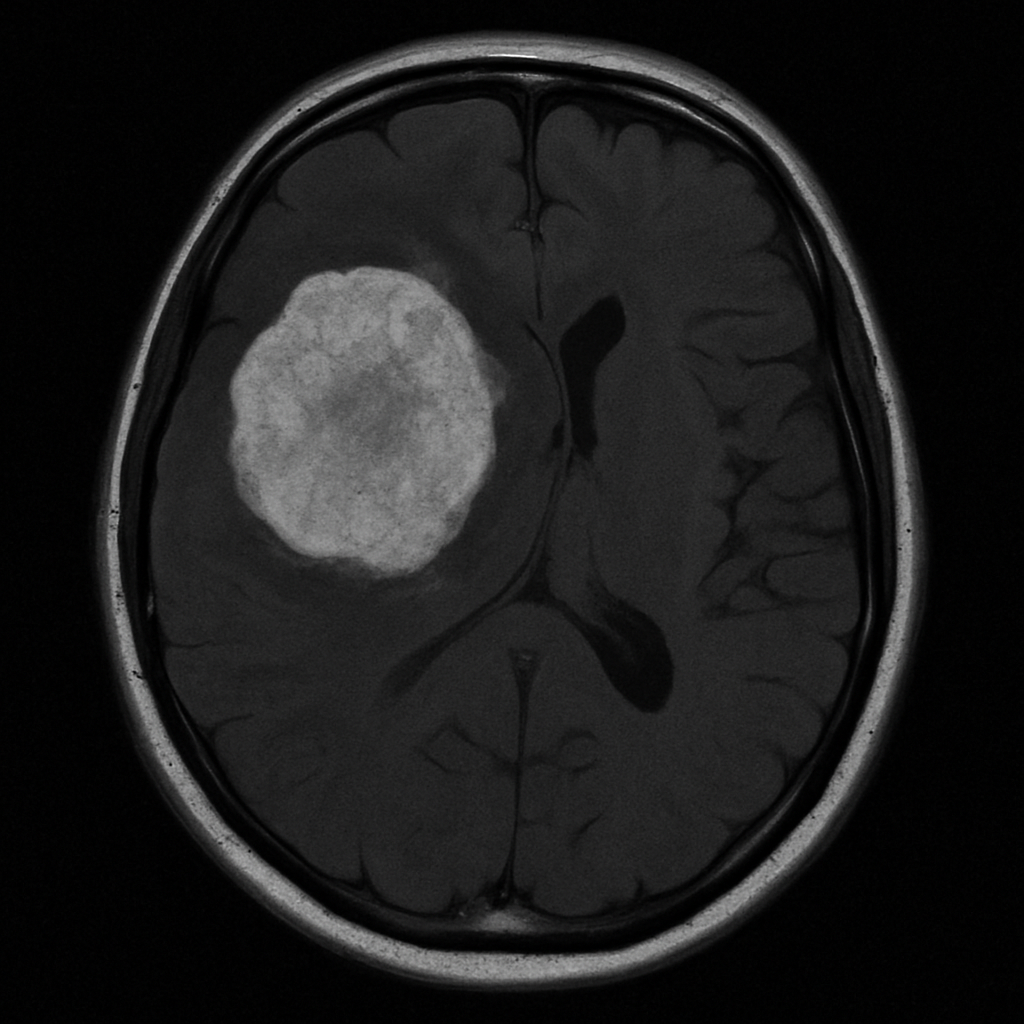
Imaging Studies
MRI and CT scans are critical in providing detailed images of the brain, helping to identify the presence, size, and location of a tumour. Advanced imaging techniques, such as functional MRI or PET scans, can offer additional insights into tumour activity and brain function.
Biopsy Procedures
A biopsy involves taking a sample of the tumour tissue to examine under a microscope. This helps determine the tumour type and grade, providing essential information for treatment planning. In some cases, a stereotactic needle biopsy may be used for hard-to-reach tumours.
Neurological Assessment
A comprehensive neurological exam assesses brain function by testing reflexes, coordination, and sensory skills. This exam helps identify specific areas of the brain affected by the tumour and guides further diagnostic and therapeutic decisions.
Genetic and Molecular Testing
Genetic and molecular testing of tumour samples can reveal specific mutations or markers that may influence treatment options. This personalized approach to diagnosis and treatment is becoming increasingly important in the management of brain tumours.
Multidisciplinary Approach
Diagnosing brain tumours often involves a team of specialists, including neurologists, neurosurgeons, radiologists, and oncologists. This collaborative approach ensures that all aspects of the tumour and its impact on the patient are thoroughly evaluated.
Treatment Options
Treatment for brain tumours depends on various factors, including the type, size, and location of the tumour, as well as the patient’s overall health. Common treatment options include:
Surgery
Surgery is often the first step in treating brain tumours. The goal is to remove as much of the tumour as possible without damaging healthy brain tissue. In some cases, surgery may be followed by other treatments to target remaining cancer cells.
Surgical Techniques
Advanced surgical techniques, such as image-guided surgery and minimally invasive approaches, have improved outcomes and reduced recovery times. Intraoperative MRI and other technologies help surgeons navigate complex brain structures.
Risks and Considerations
While surgery can be effective, it carries risks, including infection, bleeding, and neurological deficits. Careful preoperative planning and postoperative care are essential to minimize these risks and optimize recovery.
Post-Surgical Rehabilitation
Rehabilitation following surgery may involve physical therapy, occupational therapy, and speech therapy to help patients regain lost functions and improve quality of life. A multidisciplinary team approach is often used to tailor rehabilitation plans to individual needs.
Radiation Therapy
Radiation therapy uses high-energy beams to destroy tumour cells. It can be used alone or in combination with surgery or chemotherapy. This treatment is particularly useful for tumours that cannot be surgically removed.
Types of Radiation Therapy
Different types of radiation therapy, such as stereotactic radiosurgery or proton therapy, offer varying benefits based on tumour type and location. These advanced techniques allow for targeted treatment with minimal impact on surrounding healthy tissue.
Side Effects and Management
Radiation therapy can cause side effects, including fatigue, skin changes, and cognitive effects. Managing these side effects is an important part of the treatment process and involves supportive care and regular monitoring.
Combination Therapies
Radiation is often combined with other treatments, such as chemotherapy or targeted therapy, to enhance its effectiveness. This multimodal approach is tailored to the specific characteristics of the tumour and the patient’s overall health.
Chemotherapy
Chemotherapy involves using drugs to kill cancer cells. It can be administered orally or intravenously and is often used in conjunction with other treatments. While effective, chemotherapy can have significant side effects, including fatigue, nausea, and increased risk of infection.
Chemotherapy Regimens
Different chemotherapy regimens are used depending on the type and grade of the tumour. Some regimens may involve a combination of drugs to target different aspects of tumour growth and resistance.
Personalized Medicine
Advances in personalized medicine have led to the development of chemotherapy agents that target specific genetic mutations within tumour cells. This approach aims to improve effectiveness while reducing side effects.
Supportive Care During Chemotherapy
Managing the side effects of chemotherapy is crucial for maintaining quality of life during treatment. Supportive care measures, including nutritional support, anti-nausea medications, and psychosocial support, are integral to the treatment plan.
Targeted Therapy
Targeted therapy focuses on specific abnormalities within cancer cells. By targeting these specific features, this therapy can help slow or stop the growth of tumour cells while minimizing damage to healthy cells.
Mechanisms of Action
Targeted therapies work by interfering with specific molecular pathways involved in tumour growth and progression. These therapies are often used in tumours with identifiable genetic mutations or markers.
Emerging Targeted Treatments
Ongoing research is identifying new targets and developing novel therapies for various brain tumours. These emerging treatments hold promise for improving outcomes and expanding options for patients with resistant or recurrent tumours.
Integration with Other Treatments
Targeted therapy is often used alongside other treatments, such as chemotherapy or radiation, to enhance their effectiveness. This integrated approach is tailored to the unique characteristics of each patient’s tumour.
Supportive Care
In addition to these treatments, supportive care is crucial for improving quality of life. This includes pain management, physical therapy, and psychological support to help patients cope with the challenges of living with a brain tumour.
Pain and Symptom Management
Effective pain management involves a combination of medications, physical interventions, and complementary therapies. Addressing other symptoms, such as fatigue or cognitive changes, is also a key component of supportive care.
Rehabilitation and Occupational Therapy
Rehabilitation services help patients regain lost skills and adapt to changes in their abilities. Occupational therapy focuses on improving daily functioning and promoting independence.
Psychological and Emotional Support
Living with a brain tumour can be emotionally challenging for patients and their families. Access to psychological support, counseling, and support groups is essential for addressing the emotional impact of the diagnosis and treatment.
Prognosis and Survival Rates
The prognosis for brain tumours varies widely depending on the type, grade, and location of the tumour, as well as the patient’s age and overall health. While some tumours can be effectively treated or managed, others may be more challenging to treat. Early detection and advances in treatment have improved survival rates for many types of brain tumours.
Factors Influencing Prognosis
Prognostic factors include the tumour’s histology, genetic profile, and response to treatment. Age and overall health also play a role in determining the outcome. Understanding these factors helps in developing a personalized treatment plan.
Advances in Treatment
Recent advances in surgical techniques, radiation therapy, and targeted treatments have contributed to improved outcomes for many patients. Ongoing research continues to explore new approaches and therapies to further enhance survival rates.
Importance of Early Detection
Early detection of brain tumours can significantly impact treatment options and outcomes. Regular monitoring and awareness of symptoms are key to identifying tumours at an early stage, when they are more amenable to treatment.
Conclusion
Brain tumours are complex and require a comprehensive approach to diagnosis and treatment. By understanding the different types of brain tumours and their characteristics, patients and their families can make informed decisions about their care. If you or a loved one is facing a brain tumour diagnosis, it’s important to work closely with a healthcare team to explore all available options and develop a personalized treatment plan.
Understanding brain tumours is the first step in navigating the challenges they present. With ongoing research and advances in medical technology, there is hope for improved treatments and outcomes for those affected by this serious condition.
The Role of Research and Innovation
Continuous research and innovation in the field of neuro-oncology are critical for discovering new treatments and improving existing ones. Support for research initiatives and clinical trials is essential for advancing our understanding and management of brain tumours.
Empowering Patients and Families
Education and awareness empower patients and their families to actively participate in their care decisions. Access to reliable information and resources is vital for navigating the complexities of a brain tumour diagnosis.
Looking to the Future
The future of brain tumour treatment holds promise, with ongoing advancements in precision medicine, immunotherapy, and other innovative approaches. Collaboration between researchers, clinicians, and patients is key to driving progress and improving outcomes for all affected by brain tumours.
